|
|
How Society's Light Pollution affects Human Breast Cancer
Background: The pages on this website have been concerned with light pollution. So why be concerned with cancer, especially breast cancer? Well, after skin cancer, breast cancer is the most common cancer among women in the US, and it is the second leading cause of cancer death in women, after lung cancer. The following data came from the American Cancer Society's Breast Cancer Facts & Figures publications.
| Year: | 2005 | 2007 2 | 2009 | 2011 | 2013 |
|---|---|---|---|---|---|
| New cases of invasive breast cancer | 211,240 | 178,480 | 192,370 | 230,480 | 232,340 |
| New cases of CIS 1 | 58,490 | 62,030 | 62,280 | 57,650 | 64,640 |
| Deaths | 40,410 | 40,460 | 40,170 | 39,520 | 39,620 |
1 CIS
(carcinoma in situ) is non-invasive and is the earliest form of breast cancer.
2 The expected number of new breast cancers in 2007 was markedly lower than the estimate for 2005 in the previous Breast Cancer Facts & Figures report due to the use of a new, more accurate estimation method and a small decline in the breast cancer incidence rate.
American Cancer Society. Breast Cancer Facts & Figures 2005-2006. Breast Cancer Facts & Figures 2007-2008. Breast Cancer Facts & Figures 2009-2010. Breast Cancer Facts & Figures 2011-2012. Atlanta: American Cancer Society, Inc.
According to the ACS's Cancer Facts & Figures reports, the death rate of the breast cancer is going down. This is attributed to the continual messages about getting check out, finding the cancers earlier, and to better treatments.
However, it does not say that the numbers of new cases are going down.
Note that one technique to fighting cancer is to use hormone suppressant therapies
. For some types of
breast cancer, about two out of three cases are said to be hormone sensitive, for they are fueled by the hormones estrogen
or progesterone. Biopsies can reveal whether a tumor has receptors for estrogen (ER-positive) and/or progesterone (PR-positive).
And there are medications that keep the hormones from promoting further cancer growth. However, instead of society sitting around
and wait for a pill
to be one day invented that will cure breast cancer
, it seems to me that we should take action
to avoid causing it in the first place by making changes that allow our own natural suppressant abilities to work. Prevention that
we can do is an intelligent first action to take before cancer occurs.
The problem is that even weak amounts of light can impede our pineal gland from creating the beneficial
melatonin. Without melatonin, other glands produce their hormones unchecked, which lead to ever greater breast cancer rates. In our
industrialized societies, light pollution or light at nights becomes harder and harder to avoid, even if you knew to avoid it.
Everyone's impression is that it is only light
. And this apathetic acceptance may be a reason for the ever greater breast
cancer rates in industrialized societies. Technology is only good when it is properly used. So while we may herald a modern,
glitzy, flashy and hyper-lit technological society, when it threatens our health, it needs to be called into question, even if it
is just light
.
The papers that have been reviewed are reorganized by subject and by date in this listing. I have commented
on them in a chronological sequence below.
Lights at night and breast cancer risks in women
- Geographic Patterns of Breast Cancer in the U.S.
- Electric Power Use and Breast Cancer: A Hypothesis
- Inverse association between breast cancer incidence and degree of visual impairment in Finland
- Night Shift Work, Light at Night, and Risk of Breast Cancer
- Rotating Night Shifts and Risk of Breast Cancer in Women Participating in the Nurses' Health Study
- Blocking Low-Wavelength Light Prevents Nocturnal Melatonin Suppression with No Adverse Effect on Performance during Simulated Shift Work
- Melatonin-Depleted Blood from Premenopausal Women Exposed to Light at Night Stimulates Growth of Human Breast Cancer Xenografts in Nude Rats
- Light at Night Co-distributes with Incident Breast but not Lung Cancer in the Female Population of Israel.
- Light-at-night, circadian disruption and breast cancer: assessment of existing evidence
- Does the Modern Urbanized Sleeping Habitat Pose a Breast Cancer Risk?
- Circadian and Melatonin Disruption by Exposure to Light at Night Drives Intrinsic Resistance to Tamoxifen Therapy in Breast Cancer
Additional relevant information about light verses melatonin are discussed here:
- Role of pineal gland in aetiology and treatment of breast cancer.
- Two letters responded to pineal gland aetiology and breast cancer.
- Cohen, Lippman and Chabner reply to the two letters about their Pineal Gland and Breast Cancer review
- Melatonin: a potent, endogenous hydroxyl radical scavenger
Back to Light Pollution vs. Human Health
Geographic Patterns of Breast Cancer in the U.S.
Source: Journal of the National Cancer Institute, 1977, Vol. 59, p1407-1411.
William J. Blot, Joseph R. Fraumeni Jr, B. J. Stone
Environmental Epidemiology Branch, National Cancer Inst.,
National Institute of Health, Public Health Service
U.S. Dept. of Health, Education and Welfare, Bethesda, MD
The researchers calculated correlations between the mortality rates for premenopausal and postmenopausal women and demographic data for the 3,056 U.S. counties from 1950 to 1969. They found a northern predominance of the tumors in postmenopausal women and a particular high rate of breast cancer mortality in the northeast and other urban centers, but a uniform tumor distribution in premenopausal women across the country. Income status, German ethnicity and colon cancers where strong indicators for postmenopausal women, but it only partially explained the geographic distribution, this suggests an extrinsic risk factor that they did not find. Fertility patterns and ovarian cancers were more likely to be linked to premenopausal women's breast cancer, which suggests the importance of reproductive and genetic determinants.
The data told them that the mortality rates:
- Increased with urbanization across the country, only in the South were rates in large population centers not high.
- Increased with the median family income, and to a lesser extent, education levels.
- Decreased with high birth rates, especially for younger mothers (rates for 1st time mothers younger than 18 were 1/3rd the rate for 1st time mothers older than 35).
- Grew stronger for migrant groups, such as Japanese-Americans, as they westernized.
Blot, Fraumeni and Stone suggested that environmental factors lead to the changes of breast cancer risk. But
what those factors are they could only suggest temperature (because of a latitudinal gradient) or diet (because of the increased
risk due to the westernizing
of migrant groups). Their paper discusses the effect of urbanization, but a direct correlation
between increased light pollution and breast cancer risk is not mentioned, nor did it occur to the authors, then.
To help you see this effect of the light pollution concept, I have collected and tried to match the data maps from two different studies. I chose to focus on the northeastern quarter of the U.S. for it is my understanding is that the population demographics there for the study's time period did not change much, thus any demographic differences should not affect the comparison. What is difficult in the comparisons, however, is that the data maps use two different projections for their presentations.
The colorful first map below is from the light pollution study done by P. Cinzano, F. Falchi, C. D. Elvidge. ISTIL, Thiene, Italy. © 2001. Cinzano's map was presented in a cylindrical, Mercator projection as what would be viewed from a equatorial orbiting satellite. His mid-1970s data map of the same region's light pollution is the closest to the time that I can find that correlates with Blot, Fraumeni and Stone's study. Hence the more northern states in Cinzano's map appeared a bit squished. However, William Plate, Assist. Dir of FAU's Office of Comm., was very kind to stretch and warp Cinzano's map so that it would better match the authors' map. The LP and Astronomy page shows more on the growth of light pollution in U.S. and what it is projected to become in 2025.
 The second map below is the authors' greyscale mapping by county of the incidences of
postmenopausal breast cancer from 1950 to 1969. It is presented in the cartographer's point of view as would be seen from
above the U.S. In the authors' map, the darker the county, the higher the rate of incidence of breast cancers occurred. Their
greyscale legend appears to the right.
The second map below is the authors' greyscale mapping by county of the incidences of
postmenopausal breast cancer from 1950 to 1969. It is presented in the cartographer's point of view as would be seen from
above the U.S. In the authors' map, the darker the county, the higher the rate of incidence of breast cancers occurred. Their
greyscale legend appears to the right.
For the final map, I just transparently overlaid the warped Cinzano's map onto Blot's map for an immediate comparison. You should be able to see that all the colorful, bright areas of Cinzano's map pretty well matches up with the dark/high breast cancer areas of Blot's map. With a bit of thought, you should be able to recognize the East Coast corridor, find Cape Cod, the Chesapeake, the density of the cities west of Lake Michigan, the cities of Cleveland and Buffalo. You'll also note that there are cities of southern Canada that are in Cinzano's map which Blot did not cover.
This exercise shows that the higher density of breast cancer cases correlates with those areas of high
urbanization and thus high levels of light pollution. To see the different maps, just move your mouse over the maps to see how
each compares to the other.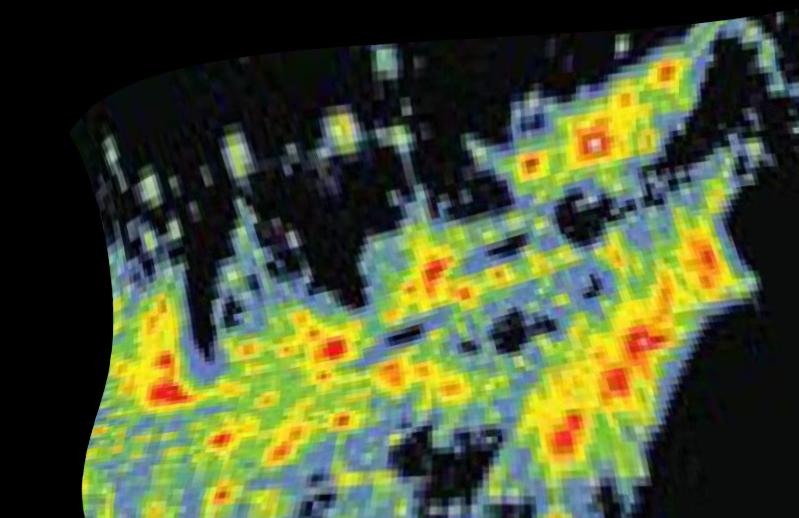
Additional credit: P. Cinzano, F. Falchi, C. D. Elvidge. Copyright 2001 ISTIL, Thiene. Reproduced from ISTIL Report 2001.
Dr. Richard G. Stevens, an epidemiologist now with the University of Connecticut's Health Center, had followed earlier papers about light and melatonin and was concerned with why breast cancers still seemed to grow in society for several decades. In 1985, he was awaken by a streetlight beaming into his apartment window. "The light was almost bright enough for me to read by," he later said, "and I thought: What about that? What about light at night?" That annoying streetlight helped make a connection about the earlier papers and the general increased light pollution throughout society was a factor for the growth of breast cancer rates, especially in industrialized areas. The next paper covered is his proposed hypothesis.
Electric Power Use and Breast Cancer: A Hypothesis
Source Link: American Journal of Epidemiology, 1987, Vol. 125, No. 4, pages 556-561.
Richard G. Stevens
(at the time of the paper:) Pacific Northwest Laboratory, Richland, WA
(currently:) Professor of Community Medicine and a Cancer Epidemiologist of the Department of Community Medicine and Healthcare,
University of Connecticut Health Center, Farmington, CT
In this paper Dr. Stevens reviewed what is known about the epidemiology of breast cancer and based on that proposed a hypothesis. He reviewed the facts and reported that:
- Large differences exist among populations in breast cancer incidences and mortality,
- Incidence rates are: low in Africa & Asia, intermediate in southern Europe and South America, and high in northern Europe and North America,
- Race does not account for the different rates, Japanese migrant studies show low rates in Japan, medium rates in Japanese in Hawaii, and high rates in Japanese in California,
- Japanese women have 1/5th the rate of US women, though they are rising as Japan "westernizes",
- Diet does not prove to be a conclusive cause of breast cancer, while rates correlate with per capita fat consumption, that appears to be a cultural coincidence, as studies show on an individual basis the risk correlation is inconclusive,
- Reductions in the pineal gland's melatonin production increases breast cancer risk,
- "Environmental lighting" can achieve that same effect, and
- Electricity provides the lighting, is used in ever greater amounts in metropolitan centers and populations in those urban settings show an increase in breast cancer risks.
So, a light went off in Dr. Stevens' head. He proposed that it is the use of electric power, either from the
lights that the electric grid powers or from the varying e-fields from the grid itself which is causing increase the risk of breast
cancer in urban cities. The hypothesis is based on experimental evidence that shows an effect of light and extremely low
frequency electric and/or magnetic (ELF) fields on pineal melatonin production, and on the relationship of melatonin to mammary
carcinogenesis.
He then covers some papers that look into partial aspects of this concept. For the electric fields he notes
an experiment on rats that used very large fields of strengths varying from 1.5 to 65 kV/m for 20 hours a day for 30 days. Due to
body shapes
, the 1.5 kV/m field should be equivalent to a 100-500 V/m field strength in humans. While there were
differences of melatonin levels between exposed rats and their controls, the field strength is well above levels populations are
routinely exposed to. He also pointed out another study, though small in scale, which failed to find a connection between cancer
mortality in those near electrical transmission lines in Britain.
However, he noted a study that showed that very low light levels, 22 nW/cm² (that is 22 Billionths of a watt per square cm!) were enough to reduce pineal melatonin production in rats. Humans have a similar response, though at somewhat higher levels.
On this basis, chronic lack of a dark night in high electric-use communities may simulate low level "constant-light", and contribute to the geographic variation in breast cancer.
He suggested that an experiment of three groups of rats be done. The first group of an electric field, the second of constant light and the last being the control where neither was done and compare the results.
Also consider this information in regards to migrant groups. The first generation that arrives to a light polluted county in the U.S. may not have had an initial light pollution exposure. As they stay in the U.S., their exposure to the light continues to affect their hormones. Subsequent generations then born in the U.S. develop in the womb of their mothers that have growing hormonal alterations. Every generation undergoes this same hormonal alteration on top of the general growing light pollution.
It was stated earlier that the pineal gland makes the melatonin, but only does so when it is dark. How dark does it have to be? Well, here is a simple rule that almost anyone can do without any specific equipment:
That's right, NO nightlights, television, nor hall lights should be left on. Windows need to curtained against intrusive outdoor light pollution sources. Clocks with their self-luminous faces, should at least glow red or use red L.E.D.s, see below. If you think that is extreme, then consider this next study of blind women in Finland.
Inverse association between breast cancer incidence and degree of visual impairment in Finland
Source Link: British Journal of Cancer, 1990, Volume 80, Number 9, pages 1459-1460.
PK Verkasalo1,2, E Pukkala3, RG Stevens4, M Ojamo5 and S-L Rudanko5
1Department of Public Health, PO Box 41, FIN-00014 University of Helsinki, Finland
2National Public Health Institute, Division of Environmental Health, P.O. Box 95, FIN-70701 Kuopio, Finland
3Finnish Cancer Registry, Liisankatu 21B, FIN-00170 Helsinki, Finland
4Pacific Northwest National Laboratory, P.O. Box 999, Richland, WA 99352, USA
5Finnish Register of Visual Impairment, Mäkelänkatu 50, FIN-00510 Helsinki, Finland
The researchers identified 10,935 women with visual impairment from the Finnish Registry and followed the women in the Finnish Cancer Registry between the years of 1983-1996. The researchers sorted the women based on degrees of visual impairment, counted up the number of years they were in the Registries, counted the number of breast cancer and other types of cancer cases in each group and compared that number with their expected cancer incident rates. They found a decrease in breast cancer rates as the visual impairment increased in the women. No similar correlation was found with the other types of cancers and in fact their rates were slightly increased. Here is the breakdown of their numbers:
| Degree of Visual Impairment | Numbers | Person-years | Observed Breast Cancers |
Cancer Incidence | Expected Breast Cancers | SIR |
|---|---|---|---|---|---|---|
| Moderate low vision | 6 440 | 32 213 | 81 | 0.2395% | 77.14 | 1.05 |
| Severe low vision | 1 896 | 9 403 | 21 | 0.2326% | 21.88 | 0.96 |
| Profound low vision | 1 538 | 8 104 | 15 | 0.2343% | 18.99 | 0.79 |
| Near-total blindness | 856 | 4 848 | 6 | 0.1875% | 9.09 | 0.66 |
| Total Blindness | 205 | 1 627 | 1 | 0.1308% | 2.13 | 0.47 |
| Total | 10 935 | 56 195 | 124 | 0.2299% | 129.17 | 0.96 |
The Expected Breast Cancer numbers comes from the cancer incidence rates of each group times their number of person-years. The SIR or the Standardized Incidence Ratios is just the Observed Breast Cancer numbers divided by the Expected Breast Cancer numbers for each group. As the less blind groups had greater numbers, their cancer incident rates approached the national average rates. However as the populations in the groups with greater visual impairment were smaller in number, their cancer incident rates would be more affected by the health of individuals in the groups. While the 50% reduction in breast cancer rates in totally blind women was based on a small numbers, it did match risk estimates from two other studies.
Thus this study found that those women with normal vision had TWICE the risk of breast cancer compared to those which were totally blind. Note that the study did not break down the sighted women by their lights-at-night exposures. Had they done so, we might have had an even clearer understanding of the risk factors.
However, the next two studies did exactly that by identifying those women who worked non-regular shifts, their sleeping conditions and whether they had breast cancer. The first study was a randomized investigation of women that were contacted via the telephone. The second study looked at women participating in a Nurse's health study. As if their jobs were not stressful or hard enough, now it seems that the light levels at their very work places, due to the times at which they work, can be cancerous.
Night Shift Work, Light at Night, and Risk of Breast Cancer
Source Link: Journal of the National Cancer Institute, Oct. 17th, 2001, Vol. 93, No. 20, pages 1557-1562.
Scott Davis1,2, Dana K. Mirick3, Richard G. Stevens4
1Program in Epidemiology, Division of Public Health Sciences, Fred Hutchinson Cancer Research
Center, Seattle, WA
2Department of Epidemiology, School of Public Health and Community Medicine, University of Washington, Seattle
3Program in Epidemiology, Division of Public Health Sciences, Fred Hutchinson Cancer Research Center
4Department of Community Medicine, University of Connecticut Health Center, Farmington.
Exposure to light at night may increase the risk of breast cancer by suppressing the normal nocturnal production of melatonin by the pineal gland, which, in turn, could increase the release of estrogen by the ovaries. This study investigated whether such exposure is associated with an increased risk of breast cancer in women. Methods: Case patients (n = 813), aged 20-74 years, were diagnosed from November 1992 through March 1995; control subjects (n = 793) were identified by random-digit dialing and were frequency matched according to 5-year age groups. An in-person interview was used to gather information on sleep habits and bedroom lighting environment in the 10 years before diagnosis and lifetime occupational history. Odds ratios (ORs) and 95% confidence intervals (CIs) were estimated by use of conditional logistic regression, with adjustment for other potential risk factors.
Results: Breast cancer risk was increased among subjects who frequently did not sleep during the period of the night when melatonin levels are typically at their highest (OR = 1.14 for each night per week; 95% CI = 1.01 to 1.28). Risk did not increase with interrupted sleep accompanied by turning on a light. There was an indication of increased risk among subjects with the brightest bedrooms. Graveyard shift-work was associated with increased breast cancer risk (OR = 1.6; 95% CI = 1.0 to 2.5), with a trend of increased risk with increasing years and with more hours per week of graveyard shift work (P = .02, Wald chi-squared test).
The results of this study provide evidence that indicators of exposure to light at night may be associated with the risk of developing breast cancer.
Rotating Night Shifts and Risk of Breast Cancer in Women Participating in the Nurses' Health Study
Source Link: Journal of the National Cancer Institute, October 17th, 2001, Vol. 93, No. 20, pages 1563-1568.
Eva S. Schernhammer1, Francine Laden1,2, Frank E. Speizer1,2, Walter C. Willett1,3, David J. Hunter1,4,5, Ichiro Kawachi1,6, Graham A. Colditz1,3,7
1Channing Laboratory, Department of Medicine, Brigham and Women's Hospital and Harvard Medical
School, Boston, MA
2Department for Environmental Health, Harvard School of Public Health, Boston
3Departments of Epidemiology and Nutrition, Harvard School of Public Health
4Department of Epidemiology, Harvard School of Public Health
5Harvard Center for Cancer Prevention, Boston
6Department of Health and Social Behavior, Harvard School of Public Health
7Epidemiology Program, Dana-Faber/Harvard Cancer Center, Boston.
Melatonin shows potential oncostatic action, and light exposure during night suppresses melatonin production. There is little information, however, about the direct effect of night work on the risk of cancer. The researchers investigated the effect of night work in breast cancer.
The researchers examined the relationship between breast cancer and working on rotating night shifts during 10 years of follow-up in 78,562 women from the Nurses' Health Study. Information was ascertained in 1988 about the total number of years during which the nurses had worked rotating night shifts with at least three nights per month. From June 1988 through May 1998, they documented 2441 incident breast cancer cases. Logistic regression models were used to calculate relative risks (RRs) and 95% confidence intervals (CIs), adjusted for confounding variables and breast cancer risk factors. All statistical tests were two-sided.
The authors observed a moderate increase in breast cancer risk among the women who worked 1-14 years or 15-29 years on rotating night shifts (multivariate adjusted RR = 1.08 [95% CI = 0.99 to 1.18] and RR = 1.08 [95% CI = 0.90 to 1.30], respectively). The risk was further increased among women who worked 30 or more years on the night shift (RR = 1.36; 95% CI = 1.04 to 1.78). The test for trend was statistically significant (P = .02).
They concluded that women who work on rotating night shifts with at least three nights per month, in addition to days and evenings in that month, appear to have a moderately increased risk of breast cancer after extended periods of working rotating night shifts.
Night-shift workers face fundamental challenges, says David Blask M.D., Ph.D., formally a Research Scientist
at the Laboratory of Chrono-Neuroendocrine Oncology, Bassett Medical Research Institute in Cooperstown, New York, now a
Professor of the Practice, the Vice Chair of the Department of
Structural & Cellular Biology at Tulane University's School of Medicine. Melatonin works, to a large degree, by inhibiting
the cancer cells from taking up linoleic acid,
he says. Cravings for fatty foods often assail workers in the middle of the
night. As a result, many shift workers consume large amounts of linoleic acid just when their melatonin production is suppressed
and unable to protect them from the polyunsaturated fat
, he says. Newer reports are showing that this greater linoleic acid
uptake, too, is becoming an additional health hazard and maybe an additional factor in the rise of obesity in industrialized
communities.
See more in the Other Health Sites section.
The next study is particularly interesting from an astronomer's point of view. Red light, those of the longest visual wavelengths, are routinely used by people to function in darkened conditions and where they do not want their developed night vision to be damaged, such as pilots flying at night or by people working in a dark room to develop old film negatives (if anyone still does that anymore!). Likewise, astronomers used it if they want to check sky charts, record notes, and such when going out to observe at night. Red light is used because shorter wavelengths, like the blue end of the spectrum, break down rhodopsin in the eyes. Rhodopsin is what our bodies make from the vitamin A rich foods we eat, like carrots, and it acts like a catalyst for our rod cells to capture photons. We need it and use it so our eyes can adjust to the dark, low level light conditions and see better. This is called our scotopic or "night vision". It is what we use to see very faint objects in the sky like galaxies or comets. Generally, it takes about thirty minutes for our eyes to build up enough rhodopsin for it to help our rod cells.
What a blue sky means to us -- Go out during the day time and look up at the blue sky. Intuitively, we know that a blue sky means that it is daytime, as it has been so for a couple of billions of years now, thanks to ancient blue-green algae generating so much atmospheric oxygen that it saturated the exposed iron (rusted them) in the rocks and then began to accumulate in the atmosphere leading to the 20% levels we have today. That oxygen refracts or scatters blue light so effectively that we just naturally assume blue skies mean daytime and would have a hard time imagining otherwise. (Which is something that potential colonists of mars will have to deal with one day! Mars' day time skies are a pale dusty orangish, only its dawn and evenings as the Sun crosses their horizon, looks bluish.)
Our brains know it. Our bodies know it. Our hormones know it. The suprachiasmatic nuclei (SCN), the center of our circadian system, knows it and responds to it. The SCN controls the pineal gland, which outputs the hormone melatonin to control the rest of our bodies. In fact, it is very the presence of the blue light that tells the SCN that it is daytime. So, in the presence of blue light, the SCN, assuming it is daytime, and acts accordingly.
In the presence of blue light, the SCN acts as if it is daytime, even if it is the middle of the night. We have just recently learned that there are some photoreceptive cells in our eyes that are neither rods nor cones, but do detect blue light and transmit that information to our suprachiasmatic nuclei. When we see this blue light, our pineal gland outputs as if it is daytime, and so then it does not create the necessary melatonin for our bodies, when we may need it.
For thousands upon thousands of generations we were hunter-gatherers, out in the daylight and exposed to that blue sky. Since about a century ago, when Edison and others developed electric lighting, we've become [a] predominantly indoor-dwelling species. We've been removed from our natural stimulus.
-- Neurologist George Brainard, Ph.D.
Director of the Light Research Program at Thomas Jefferson University, in Philadelphia.
The next study looks more carefully at simple ways to prevent blue light, or "low wavelength light", from interfering with our bodies' ability to make melatonin. After reading about it, then consider the number of people that go to bed with a light or a nightlight or a TV on. Blue light is damaging. Read the study (not just the summary offered here) and you'll find how quickly our bodies try to restore the level of melatonin in our system, once dark conditions resume, hence it seems that melatonin is quite important to our bodies. It also seems that rats cannot do that. For once their melatonin levels drop due to a bright light source, the level stays down for the rest of the night. They are also more sensitive to smaller changes of light than humans. So for all the damaging affects lights at night causes us, they probably suffer a larger impact. Now I am not about to create a pity page for rats mind you, however, it does call into question the concept of how much light pollution affects other animal species. I will try to go into greater detail about that in the light pollution verses nature pages.
Personally, I would not have used the term "low-wavelength light" to describe the shorter wavelengths of
blue light, it is a bit confusing and the title's double negative needs decoding to something more like Blocking Shorter
Wavelength Light Allows for Melatonin Secretion Without Adverse Effects on Performance during Simulated Shift Work
. However,
there it is.
Blocking Low-Wavelength Light Prevents Nocturnal Melatonin Suppression with No Adverse Effect on Performance during Simulated Shift Work
Source Link: The Journal of Clinical Endocrinology & Metabolism, 2005, Vol. 90, No. 5, pages 2755-2761.
Leonid Kayumov1,2, Robert F. Casper3, Raed J. Hawa1,2, Boris Perelman1, Sharon A. Chung1, Steven Sokalsky1, and Colin M. Shapiro1,2,4
1Sleep Research Laboratory, University Health Network, Toronto, Ontario, Canada M5T 2S8
2Departments of Psychiatry, University of Toronto, Toronto, Ontario, Canada M5T 2Z9
3Departments of Obstetrics and Gynecology, University of Toronto, Toronto
4Departments of Ophthalmology, University of Toronto, Toronto
Decreases in melatonin production in human and animals are known to be caused by environmental lighting, especially short-wavelength lighting (between 470 and 525 nm). The researchers investigated the use of goggles, which excludes wavelengths shorter than 530 nm, could prevent the suppression of melatonin in bright-light conditions during a simulated shift-work experiment. Salivary melatonin levels were measured under dim (<5 lux), bright (800 lux), and filtered (800 lux) light at hourly intervals between 2000 and 0800 h in 11 healthy young males and eight females (mean age, 24.7 ± 4.6 year). The measurements were performed during three nonconsecutive nights over a two week period. Subjective sleepiness was measured by self-report scales, whereas objective performance was assessed with the Continuous Performance Test. All subjects demonstrated preserved melatonin levels in filtered light similar to their dim-light secretion profile. Unfiltered bright light drastically suppressed melatonin production. Normalization of endogenous melatonin production while wearing goggles did not impair measures of performance, subjective sleepiness, or alertness.
This next paper is really interesting. The researchers used blood from women who were either recently exposed to light or from those who stayed in darkened conditions, and found that the different blood samples caused significantly different growth rates in breast cancer tumors. Note the rate difference is between blood taken from a women after being exposed light compared that blood from a women kept in dark conditions. Then note how similar that rate difference is with Kloog, et al, 2008, study from the Univ. of Haifa in Israel that is mentioned later on.
Melatonin-Depleted Blood from Premenopausal Women Exposed to Light at Night Stimulates Growth of Human Breast Cancer Xenografts in Nude Rats
Source Link: Cancer Research, Dec. 1st 2005, Vol. 65, No. 23, p11174-11184.
David E. Blask1, George C. Brainard2, Robert T. Dauchy1, John P. Hanifin2, Leslie K. Davidson1, Jean A. Krause1, Leonard A. Sauer1, Moises A. Rivera-Bermudez3, Margarita L. Dubocovich3, Samar A. Jasser2, Darin T. Lynch1, Mark D. Rollag4 and Frederick Zalatan1
1Laboratory of Chrono-Neuroendocrine Oncology, Bassett Research Institute, The Mary Imogene Bassett
Hospital, Cooperstown, New York
2Department of Neurology, Thomas Jefferson University, Philadelphia, Pennsylvania
3Department of Molecular Pharmacology and Biological Chemistry, Northwestern University Feinberg School of Medicine,
Chicago, Illinois
4Department of Anatomy, Physiology, and Genetics, Uniformed Services University of the Health Sciences, Bethesda,
Maryland
The scientists in report, including the same David Blask quoted above, put MCF-7 cells into mice to generate human breast cancer tumors. These tumors were then grafted into rats. (Their technique created a growing human-derived tumor with a single artery into and a single vein from the tumor. This made the tumor very controllable for the experiment.) The scientists then gave the rats blood taken from women during the day, in the earliest hours of the morning (as in 1 am to 3 am), and after being exposed to about five minutes of light at night. This last test simulated the amount of time it may take someone to turn on the light when using a bathroom. The blood that was taken during darkness and then injected into the grafts slowed the growth of the cancers by 80 percent. However, the blood taken after exposure to light, whether the light was from daytime or just from lights at night, did not slow it down at all.
The next study achieves what I crudely tried to show with Blot's 1977 Geographical Patterns of Breast Cancer study and Cinzano's 2001 Light Pollution Atlas. It shows a correlation between the high incidence of breast cancers in the overly lit cities of Haifa and Tel-Aviv. In fact the light pollution levels were the strongest factors in the correlations found. As was expected, no similar corresponding relation was found for lung cancer rates.
Again compare the breast cancer rates of the light polluted areas with those in darker areas here in the Israel study. Then note how similar this comparison is to the change in the cancer growth rates found in the Blask, et al 2005 study.
Light at Night Co-distributes with Incident Breast but not Lung Cancer in the Female Population of Israel.
Kloog, Itai1, Haim, Abraham2, Stevens, Richard G.3, Barchana, Micha4,5, Portnov, Boris A.1
1Department of Natural Resources & Environmental Management, University of Haifa, Haifa, Israel.
2Department of Biology, University of Haifa-Oranim, Kiryat Tivon, Israel.
3University of Connecticut Health Center, Farmington, Connecticut, USA.
4School of Public Health, University of Haifa, Haifa.
5Israel National Cancer Registry, Ministry of Health, Jerusalem, Israel.
Recent studies of shift-working women have reported that
excessive exposure to light at night (LAN) may be a risk factor for breast cancer. However, no studies have yet attempted to examine
the co-distribution of LAN and breast cancer incidence on a population level with the goal to assess the coherence of these earlier
findings with population trends. Coherence is one of Hill's criteria
(actually, viewpoints) for an inference of causality.
Nighttime satellite images were used to estimate LAN levels in 147 communities in Israel. Multiple regression analysis was performed
to investigate the association between LAN and breast cancer incidence rates and, as a test of the specificity of our method, lung
cancer incidence rates in women across localities under the prediction of a connection with breast cancer but not lung cancer. After
adjusting for several variables available on a population level, such as ethnic makeup, birth rate, population density, and local
income level, a strong positive association between LAN intensity and breast cancer rate was revealed (p < 0.05), and this
association strengthened (p < 0.01) when only statistically significant factors were filtered out by stepwise regression analysis.
Concurrently, no association was found between LAN intensity and lung cancer rate. These results provide coherence of the previously
reported case-control and cohort studies with the co-distribution of LAN and breast cancer on a population basis. The analysis
yielded an estimated 73% higher breast cancer incidence in the highest LAN exposed communities compared to the lowest LAN exposed
communities.
Light-at-night, circadian disruption and breast cancer: assessment of existing evidence
Source Link: Int. J. Epidemiology, August 2009, Vol. 38, No. 4, pages 963-970; doi:10.1093/ije/dyp178
Richard G. Stevens
Dept. of Community Medicine, University of Connecticut Health Center, Farmington, CT
Dr. Stevens states that the predictions include that
- Non-day shift work would increase risk (in fact the International Agency for Research on Cancer classified shift work as a probable human carcinogen).
- Blind women would be at lower risk for breast cancer.
- Long sleep duration would lower risk.
- Light level in bedrooms at night would be directly associated with risk.
- Community nighttime light level would show associations with breast cancer incidence on the population level.
Stevens also points out that one should not just take melatonin as a supplement either. While supplements can
beneficially slow the growth of an existing tumor, he points out a study have shown that melatonin can cause a phase shift to their
sleeping cycle, thus causing a circadian disruption instead of alleviating it
. This is more than just that a person's body
clock will shift the time it will want to go to sleep, such as when a person experience jetlag. So, it is best to seek the advice
of a physician before starting your own treatment.
Dr. Stevens has appeared on the CBSNews Morning Show in Nov 30th, 2007 to explain more about this problem.
Here is what I think is very exciting about this, of all the things that we do that can contribute to cancer rates, this is the easiest to correct. There are no gums to chew, patches to wear, daily workout routines to follow, or extra helpings of vegetables to eat to solve this problem. Just turn the lights off until you cannot see your hand. Especially avoid bluish lights. Replace lights that produce glare to that sleep can give you, and some neighbor down the road, all the health effects it can. And let's face it, our schedules are very filled up nowadays. Can we really afford NOT to get the most benefits of what we can out of our sleep time?
Does the Modern Urbanized Sleeping Habitat Pose a Breast Cancer Risk?
Kloog, Itai1,4, Portnov, Boris A.1, Hedy S. Rennert2, Haim, Abraham3
1Department of Natural Resources and Environmental Management, Graduate School of Management,
University of Haifa, Haifa, Israel.
2Department of Community Medicine and Epidemiology, Carmel Medical Center and Bruce Rappaport Faculty of Medicine,
Technion-Israel Institute of Technology and Clalit Health Services National Cancer Control Center, Haifa, Israel.
3The Israeli Center for Interdisciplinary Research in Chronobiology, University of Haifa, Haifa, Israel.
4Department of Environmental Health-Exposure, Epidemiology and Risk Program, Harvard School of Public Health, Boston,
Massachusetts, USA.
In this paper, the authors have investigated a relationship between the lighting levels in the bedroom, the
sleeping habitat
, and the rates of breast cancer in 1679 women. From the abstract: the novelty of the present research
is that, to the best of the authors' knowledge, this is the first study to have identified an unequivocal positive association
between bedroom-light intensity and a breast cancer risk.
Two earlier studies have also looked into this issue. In a 2001 paper, Davis and his colleagues interviewed
813 cancer patients and 793 control subjects, during 1992 and 1995, on their sleep habits and conditions in the bedroom for the 10
years before their diagnosis. When they adjusted for other potential risk factors, they did find a significantly higher breast
cancer risk factor with those subject with disturbed sleep, but not a clear association between light intensity and breast cancer
then. In a 2006 paper, O'Leary and colleagues interviewed 576 women with cancer and 585 control subjects about their
Lights-at-night
(or "LAN") exposures at work and home. Their questions included sleeping duration, frequency of lights
being turned on at night and how long they were on. While they did not ask questions regarding the intensity of the lights, they
still did find an increased breast cancer risk associated with the frequency of lights being turned on.
Since then, electricity consumption and lighting levels worldwide continue to increase. Newer outdoor high-intensity discharge lamps and more fluorescent lamps emitting bluer wavelengths are being used. So if there is a LAN-breast cancer connection, this linkage will have strengthened.
Since 2000, a questionnaire from the Breast Cancer in Northern Israel
study has been given to women in
Isreal and all women with breast cancers have been invited to participate in the study. Since 2006, it has added questions in which
participates rate their bedroom light levels at night as being either completely dark, low, average or very strong with all lights
being switched on. Other questions asked about alcohol consumption, number of births, religion, age, and education.
In this paper, the authors used the questionnaire responses, randomly sampled, of 794 breast cancer patients and 885 control participants, randomly selected, via Clalit Health Studies, a health care provider in Israel. The data analysis shows a trend in the percentages of women with breast cancers to increase with stronger lighting levels in bedrooms at night, while it decreases with the control participates. This trend was found to be the strongest predictor for breast cancer. The trends are better shown by calculating the ratios of the percentages of each group for their lighting levels. Thus, the case percentages divided by the control percentages for each lighting level becomes 0.859 for no lights, 1.055 for low light levels, 1.009 for average levels and 1.305 for the very strong levels.
While the study is limited by the need to precisely measure the lighting levels, duration and their spectra in the bedrooms, instead of depending on a questionnaire, its large size helps correct for this limitation. This study is an excellent argument for more precise future studies and for anyone to take their own preventative steps against a possible onset of cancer.
Circadian and Melatonin Disruption by Exposure to Light at Night Drives Intrinsic Resistance to Tamoxifen Therapy in Breast Cancer
Source Link: Cancer Research, 2014, August 1, Volume 74, Issue 15, doi:10.1158/0008-5472.CAN-13-3156.
Robert T. Dauchy1,4, Shulin Xiang1,3,4, Lulu Mao1,3,4, Samantha Brimer2, Melissa A. Wren1,4,5, Lin Yuan1,4, Muralidharan Anbalagan1,4, Adam Hauch2,4, Tripp Frasch1, Brian G. Rowan1,3,4, David E. Blask1,3,4, and Steven M. Hill1,3,4
1 Departments of Structural and Cellular Biology and
2 Departments of Surgery, Tulane University School of Medicine;
3 Tulane Cancer Center and Louisiana Cancer Research Consortium;
4 Tulane Circadian Cancer Biology Group; and
5 Department of Comparative Medicine, Tulane University, New Orleans, Louisiana
Artificial light at night turns off our natural production of the hormone melatonin. This new research, by Tulane University School of Medicine's cancer researchers and published in the journal Cancer Research, has found that it also makes breast cancer resistant to tamoxifen, a widely used drug to fight breast cancer, in animal tests. This is the first study that shows that melatonin, the hormone of darkness, is vital to the success of tamoxifen in treating breast cancer.
Principal investigators and co-leaders of the Tulane University Circadian Cancer Biology Group, Steven Hill and David Blask, along with team members Robert Dauchy and Shulin Xiang, investigated the role of melatonin on the effectiveness of tamoxifen in combating human breast cancer cells implanted in rats.
In the first phase of the study, the researchers kept the animals in a daily light/dark cycle of 12 hours
of light followed by 12 hours of total darkness (melatonin is elevated during the dark phase) for several weeks,
says Hill.
Then they split the animals into a group of either those to be exposed to extremely dim light at night ("dLEN" which was roughly
equivalent to faint light coming under a door or through a window from a distant streetlight) to suppress their natural melatonin
levels or into a group that continued the light-dark 12 hour:12 hour routine. They implanted MCF-7 human breast tumors into the
animals at Day Zero and watched from there. Around Day 15, the breast cancer tumors were measureable in the dLEN group and they grew
at a rate of 0.73 grams/day which was 2.6 times faster than those animals under the LD 12:12 lighting pattern (0.28 grams/day).
When they gave the animals tamoxifen, the dLEN group hardly slowed down at all (0.69 grams/day) while the LD 12:12 groups' tumors
got smaller, at the rate of -0.14 grams/day.
In the second study, the researchers exposed the animals to the same daily light/dark cycle; however, during the 12 hour dark phase, all animal groups were exposed to extremely dim light at night, again to suppress their natural melatonin levels. These animals were again split into groups in which one group was kept in those same conditions, or in another group which was injected with melatonin. The melatonin by itself delayed the formation of tumors and significantly slowed their growth but tamoxifen caused a dramatic regression of tumors in animals with either high nighttime levels of melatonin during complete darkness or those receiving melatonin supplementation during dim light at night exposure.
These findings have potentially enormous implications for women being treated with tamoxifen and also regularly exposed to light at night due to sleep problems, working night shifts or exposed to light from computer, TV screens or exterior streetlights.
High melatonin levels at night put breast cancer cells to 'sleep' by turning off key growth mechanisms.
These cells are vulnerable to tamoxifen. But when the lights are on and melatonin is suppressed, breast cancer cells 'wake up' and
ignore tamoxifen,
Blask says.
Dr. Hill wants to move the research into human breast tissue. He added a warning about using technology,
which tends to produce blue light wavelengths that disrupt melatonin production, in the run-up to bedtime. He said If you get
seven hours sleep at night, but use an iPad or computer or watch TV then those blue wavelengths are suppressing melatonin production
for anywhere from an hour to an hour and half. So instead of seven hours of melatonin, you're getting six or five and a half.
The study could make light at night a new and serious risk factor for developing resistance to tamoxifen and other anticancer drugs and make the use of melatonin in combination with tamoxifen, administered at the optimal time of day or night, standard treatment for breast cancer patients.
See also Tulane University's Press Release of the Study or this news report at: www.wwltv.com. If you wish to donate funds to aid this research, Tulane University has set up a way to do so at: http://tulane.edu/som/cancer/circadianbiologydonations.cfm.
When I think about the term "light pollution", I know that it sounds extreme. However, when one considers the damaging effects it causes us and the animals out in the wild, one realizes that light pollution is just as damaging as a toxic chemical spill across the land. The results are almost the same. The difference is that with light pollution, we keep paying for and consuming energy resources, night after night, just to re-make this very same pollution, which we could so easily correct if we just put in some effort. In short, stop harming yourself and others in society. Just turn the lights off.
Florida Atlantic University
Boca Raton, Florida
E-mail: evandern at fau dot edu
Phone: 561 297 STAR (7827)